Colorectal Case 5
Prof. Yutaka Saito
Scope: CF-EZ1500D, CF-H290ECI
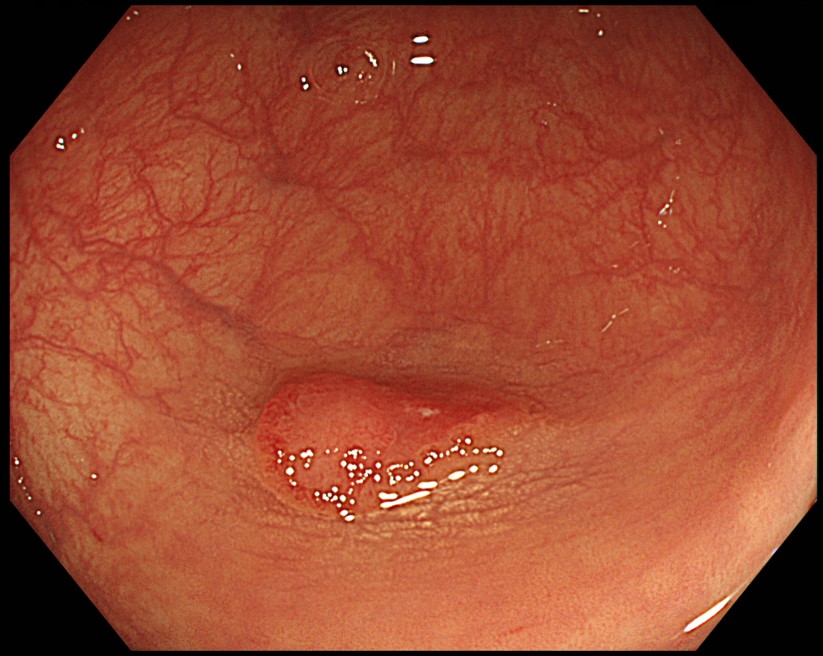
Case: 0-IIa + IIc (LST-NG), S/C, 15 mm, JNET type 2B, highly irregular pit pattern type VI (invasive pattern), cT1b
Organ: Sigmoid colon
Patient information: F, 79
Medical history: Nothing worth noting
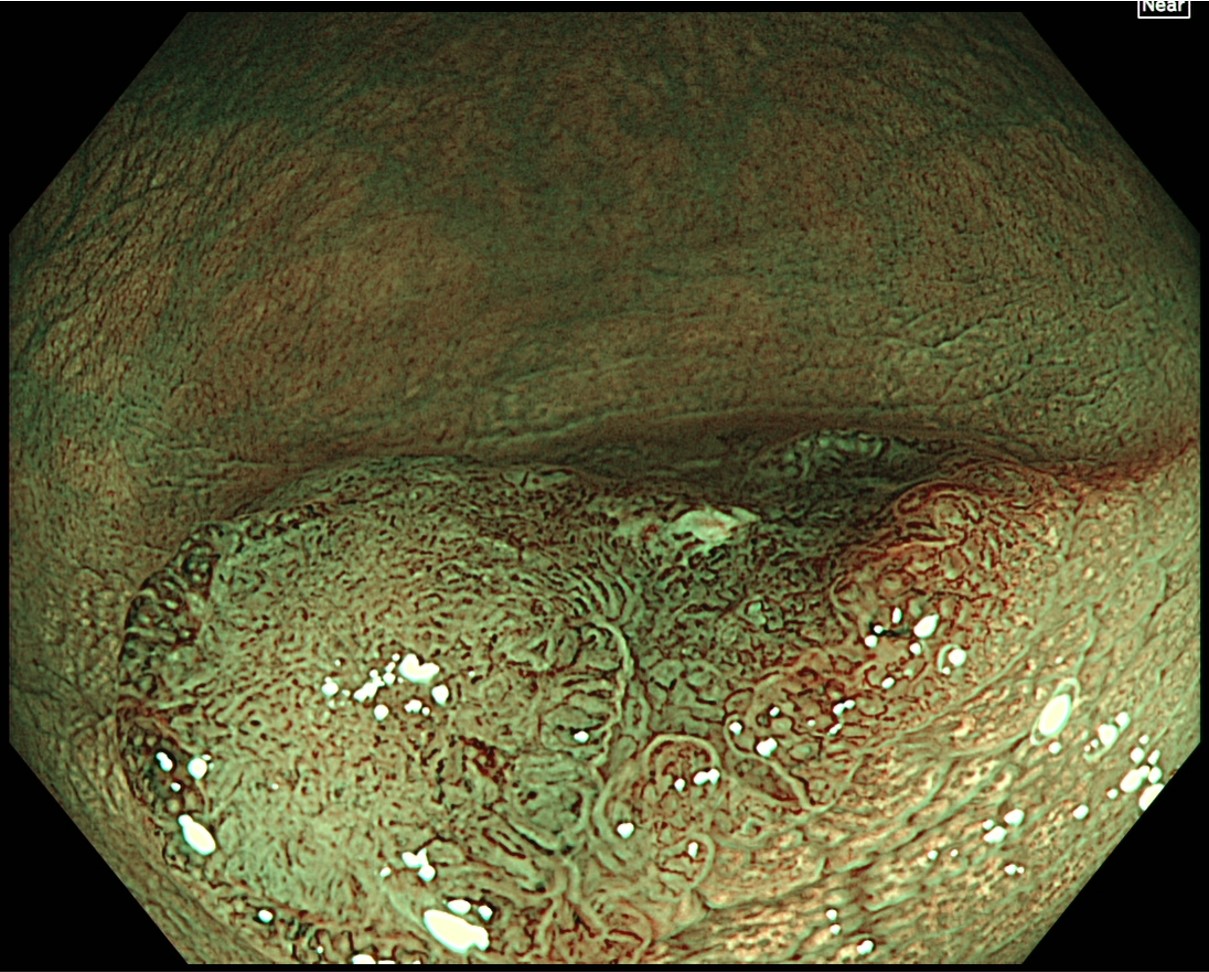
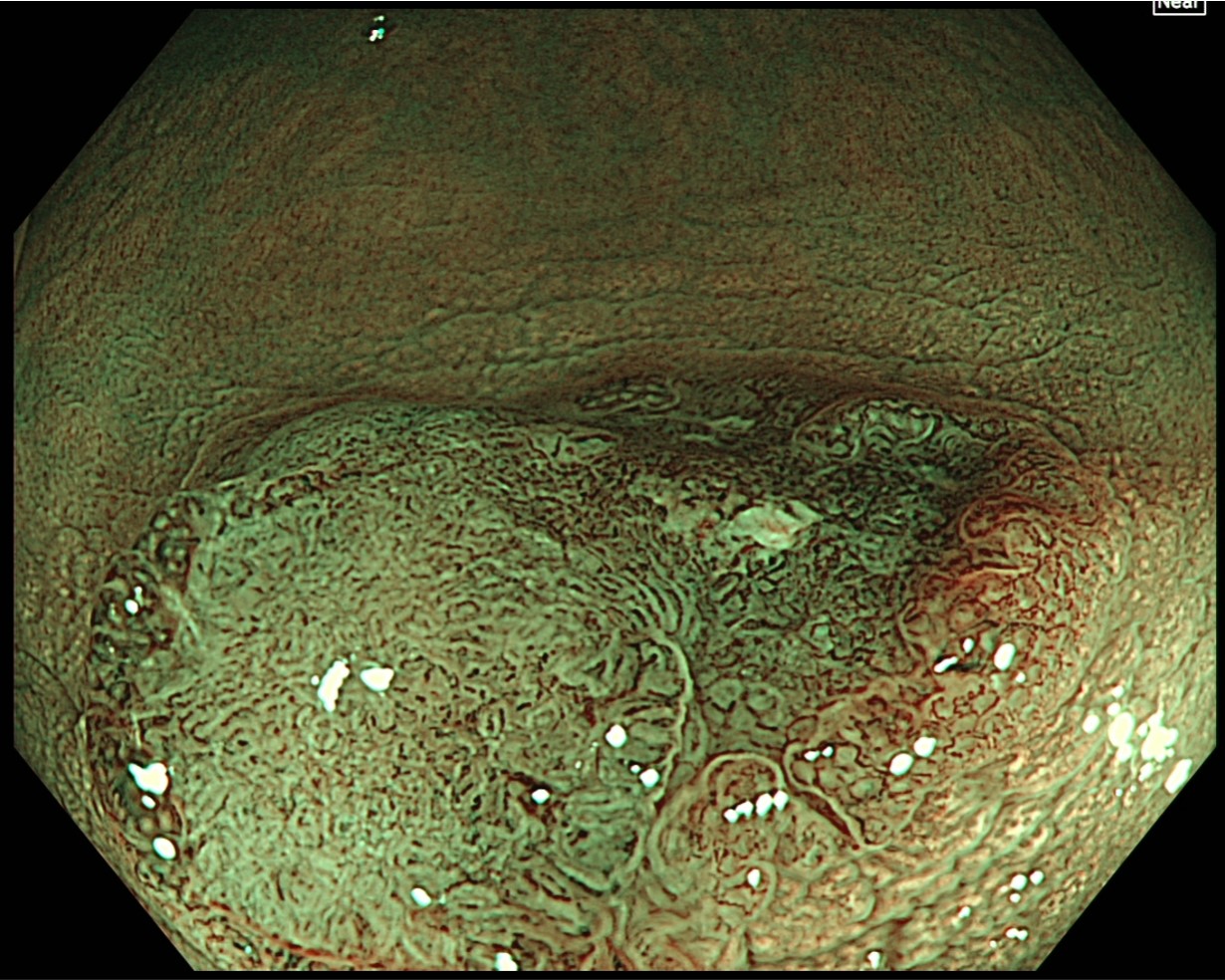
TXI “Mode 1” magnifying observation in Near Focus mode
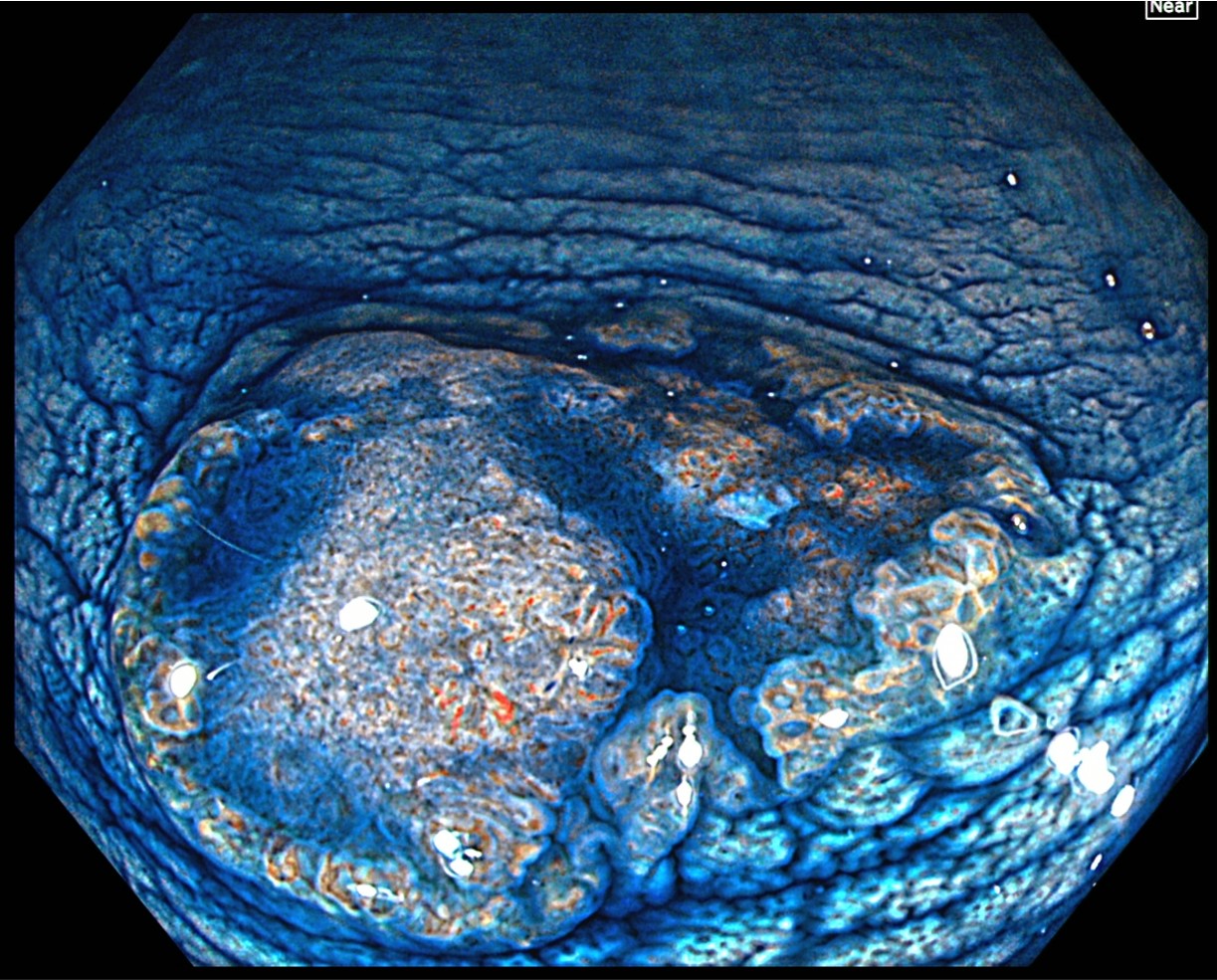
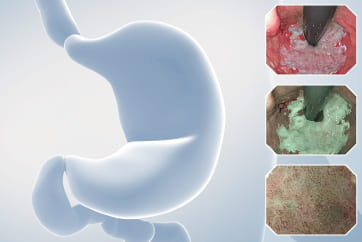
After spraying indigo carmine, magnifying observation is performed in TXI and Near Focus modes. The indigo carmine spraying clarifies the margin of the depressed area. The right side of the depressed area, which exhibits the characteristics of JNET type 2B, can be recognized as a deeper depression with a greater height difference than the left side.
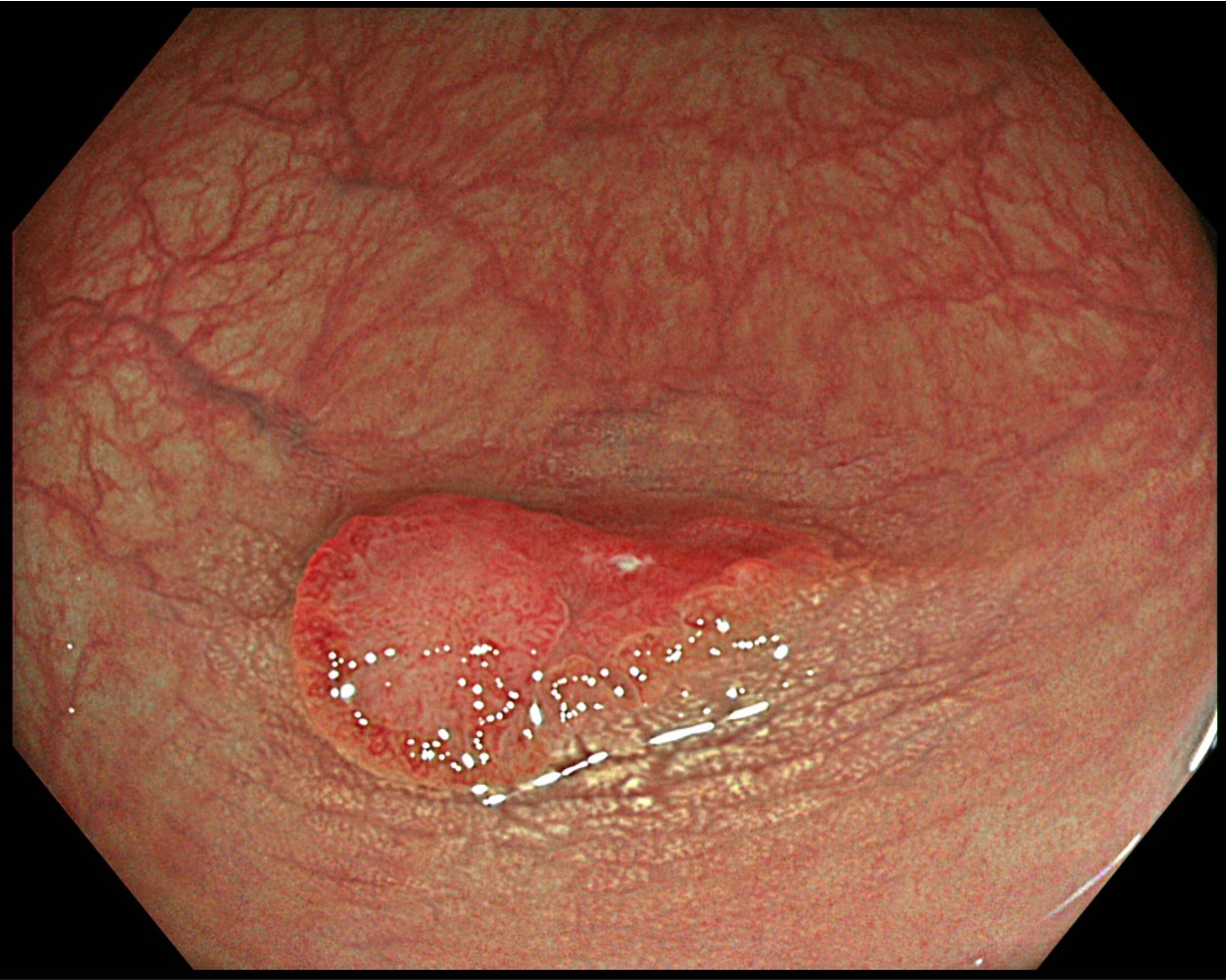
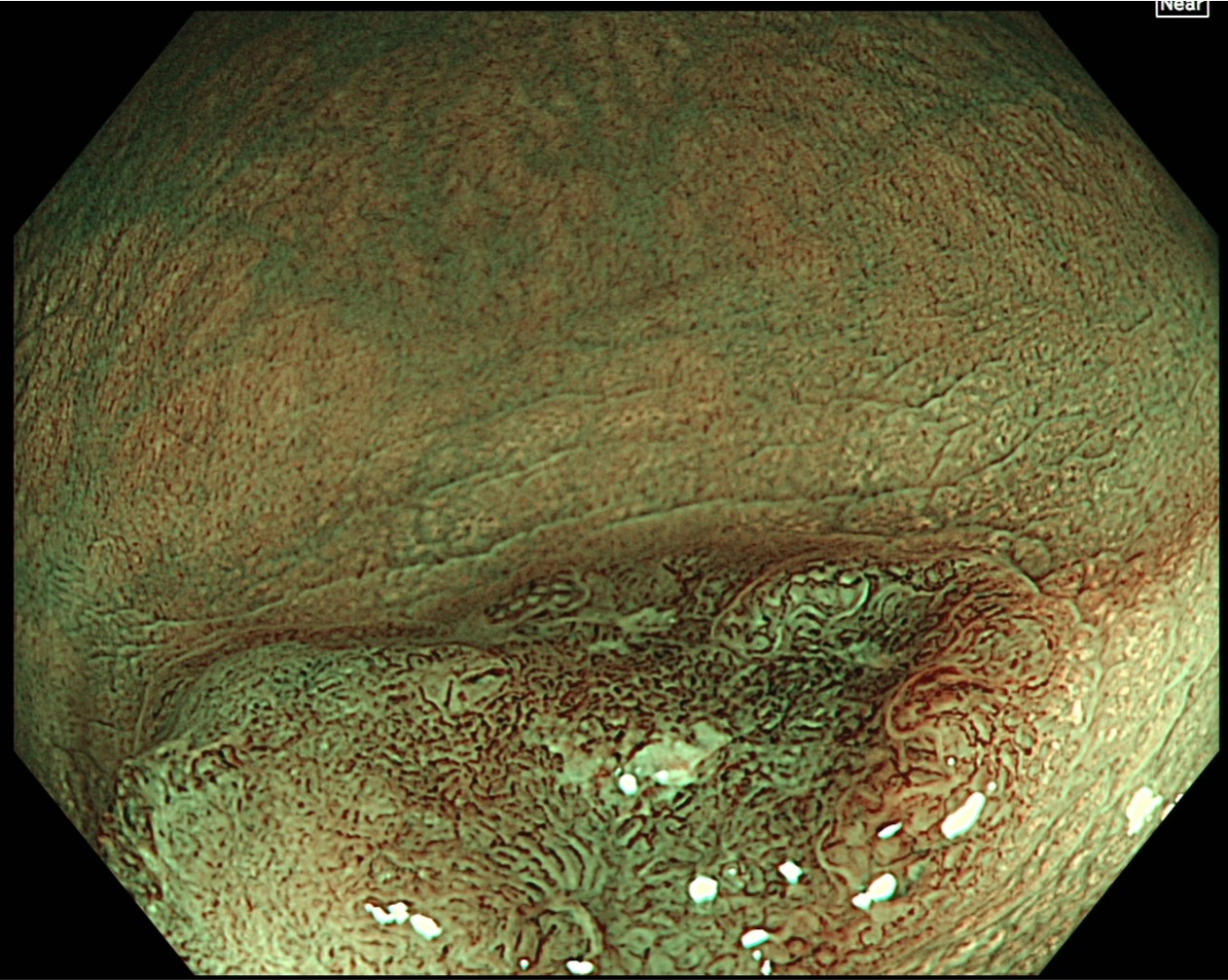
TXI “Mode 1” magnifying observation in Near Focus mode
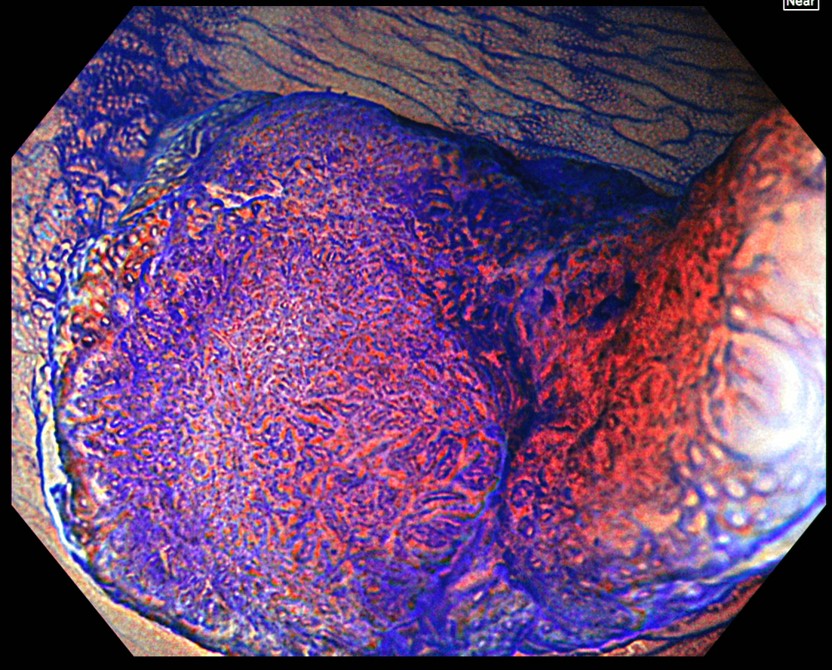
After staining with crystal violet, magnifying observation is performed in TXI and Near Focus modes. While the left side of the depressed area is classified as JNET type 2A, the margin of the left side features slightly irregular type IIIS-VI pit patterns. The region near the center is diagnosed as type VI highly irregular.
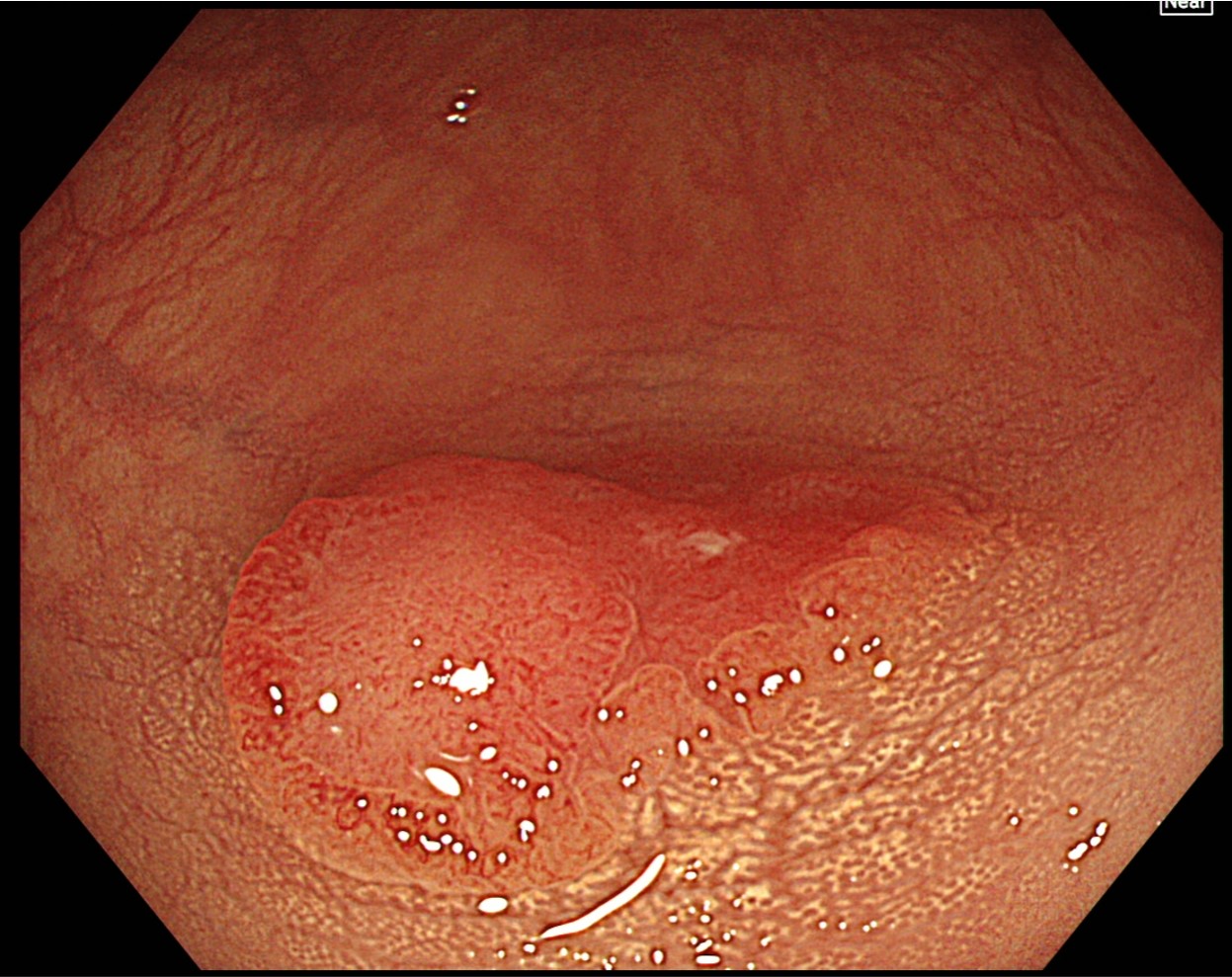
TXI “Mode 2” magnifying observation in Near Focus mode
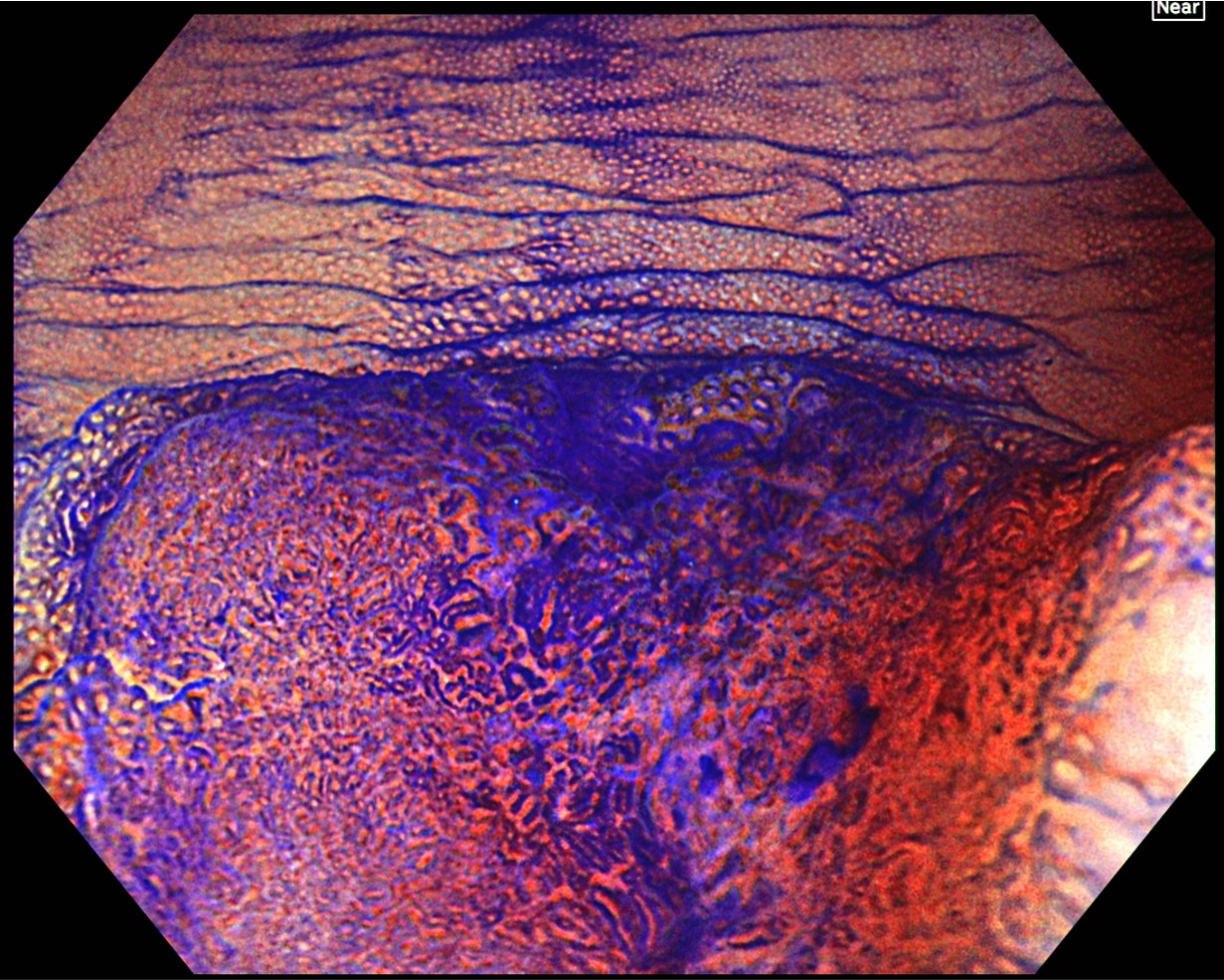
After staining with crystal violet, magnifying observation in TXI and Near Focus modes is performed. The region from the center of the depression to the right side is diagnosed as type VI highly irregular pit patterns, while the margin on the left side of the depression mainly exhibits type IIIS. The final diagnosis is 0-IIa + IIc (LST-NG), Rb, 15 mm, JNET type 2B, and type VI highly irregular pit pattern (invasive pattern), as well as cT1b cancer.
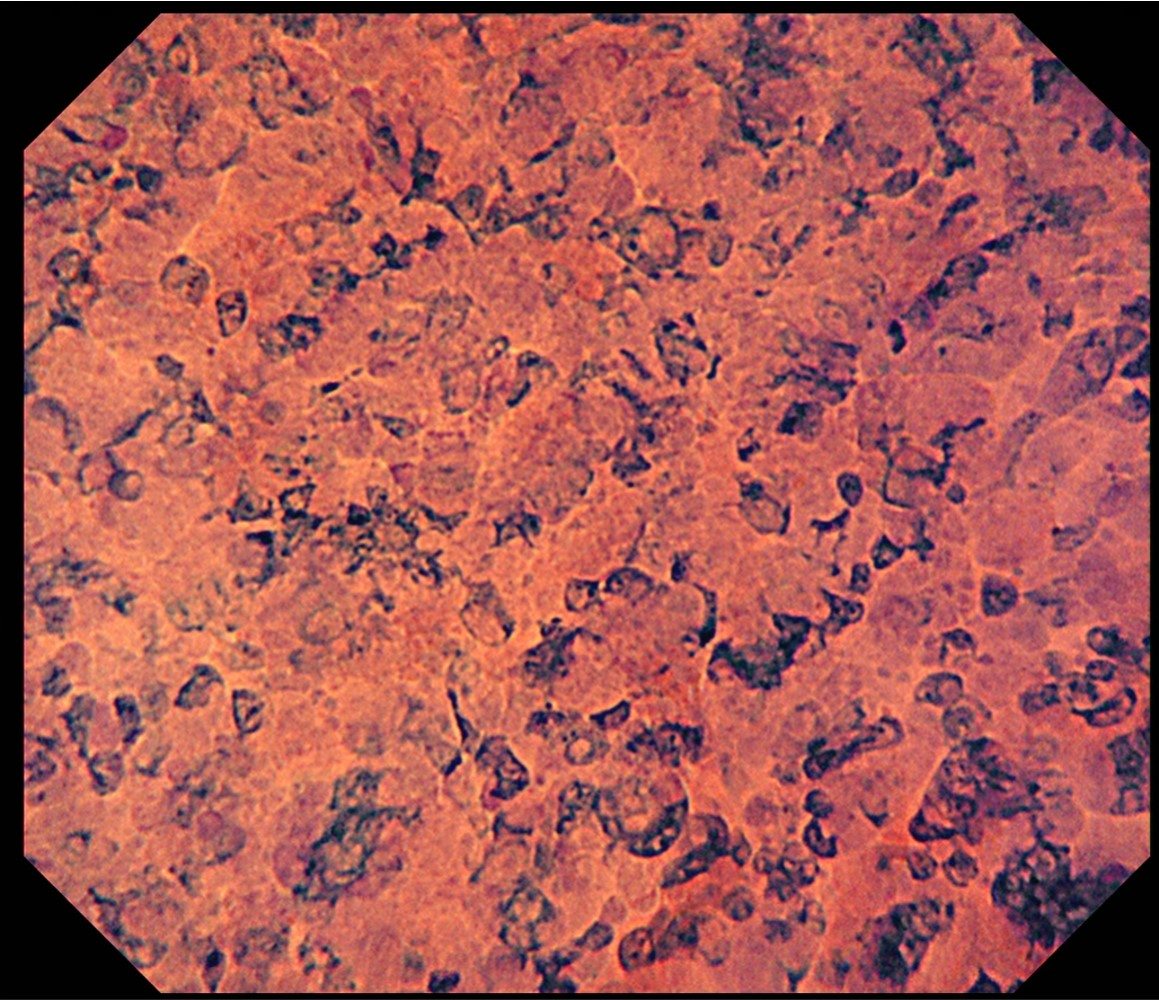
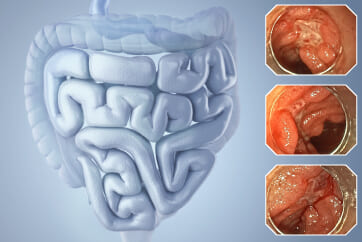
Magnifying observation after double spraying with crystal violet and methylene blue
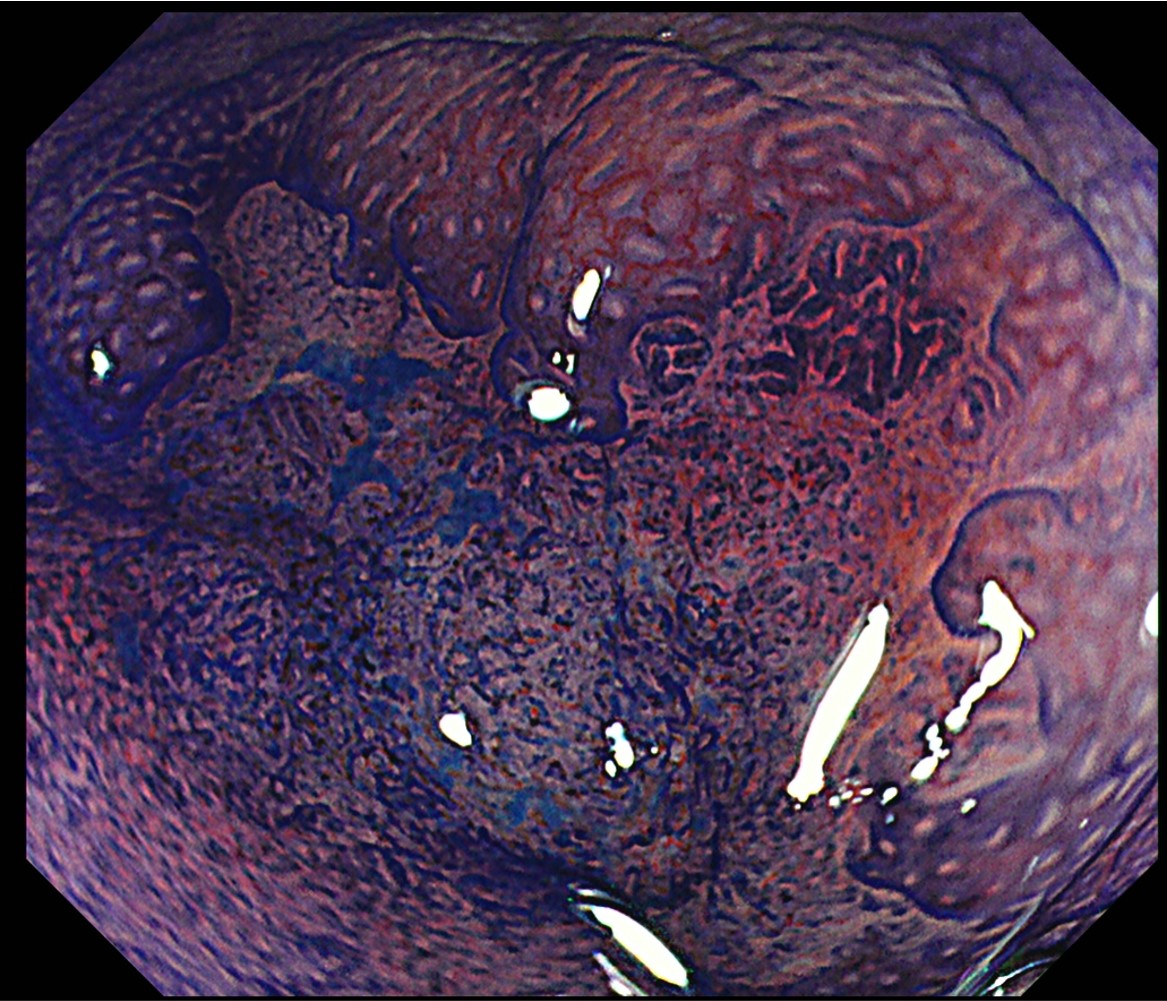
This is magnifying observation after double staining with crystal violet and methylene blue using the CF-H290ECI. Type VI highly irregular pit patterns with field cancerization can be recognized, so the lesion can be diagnosed as type VI (invasive pattern).
Case video
Surveillance colonoscopy, 0-2A + 2C (LST-NG)
The patient was a 79-year-old female. The results of the checkup she had undergone showed a positive FOBT, and a colonoscopy was performed. An early cancer was found in the sigmoid colon, and she was referred to us for endoscopic treatment.
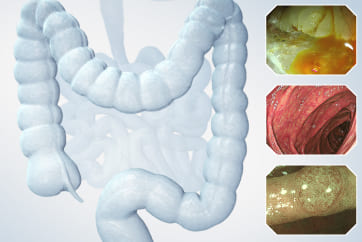
After carefully washing the site using a water jet, we started the examination. We first performed WLI, TXI, and NBI non-magnifying observation. We found the lesion in the 6 o’clock direction and switched to NBI magnifying observation in Near Focus mode.
Moving on to chromoendoscopy, we sprayed indigo carmine carefully from the proximal side of the lesion. Then we performed WLI magnifying observation in Near Focus mode. To further enhance visibility, we engaged the TXI mode.
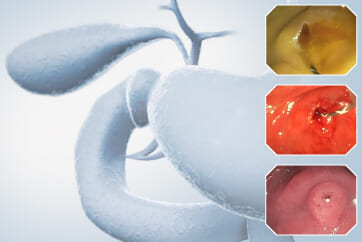
To stabilize the lesion so that we could capture clear, in-focus images, we carefully placed a non-traumatic tube on the proximal side of the lesion. The site with was carefully washed with pronase, we fed crystal violet dye through the tube. The site was stained for about 1 minute and then washed with pronase again. Water immersion observation enabled us to get clear images without halation.
Upon examination, we found that pit pattern and JNET classifications differed between the left and right sides of the depression. Consequently, we performed colonoscopy again — this time using the CF-H290-ECI scope. Following NBI magnifying observation and magnifying chromoendoscopy with indigo carmine, we performed crystal violet-stained magnifying endoscopy. Under ultra-magnification, we made sure to get images that would allow us to make 1:1 comparisons with pit patterns.
Overall Comment
The patient was a 79-year-old female. During a medical checkup, she had a fecal occult blood test which came up positive. A colonoscopy was performed, and an early cancer was detected. She was subsequently referred to us for treatment.
Under WLI non-magnifying observation, we recognized a 15-mm reddish flat lesion in the sigmoid colon. The lesion was surrounded by white spots. Under NBI observation in Near Focus mode, we observed that the normal mucosa around the lesion appeared brownish and the “O-ring” sign was positive. A depressed region was clearly visible. The redness of the lesion was further enhanced under TXI “Mode 1” standard observation.
Under NBI magnifying observation in Near Focus mode, the right side of the depression exhibited irregular vessel and surface patterns and was diagnosed as type 2B, while the left margin was considered to approximate type 2A, according to the JNET classification.
Under TXI magnifying observation in Near Focus mode, the margin of the depression was demarcated by spraying indigo carmine dye. The right side of the depression, which exhibited type 2B characteristics according to the JNET classification, had a greater height difference, so it was clearly deeper.
After staining the region on the left side of the depression — classified as JNET type 2A — with crystal violet, type IIIS-VI slightly irregular pit patterns were observed, while the region near the center was diagnosed to have type VI highly irregular pit patterns. In addition, the area extending from the center of the depression to the right side was diagnosed to have type VI highly irregular pit patterns.
Consequently, the final diagnosis was 0-IIa + IIc (LST-NG), S/C, 15 mm, JNET type 2B, highly irregular pit pattern type VI (invasive pattern), and cT1b cancer. When we performed additional magnifying observation using the CF-H290ECI, highly irregular pit patterns with field cancerization were likewise confirmed, leading to diagnosis of type VI (invasive pattern). Also in ultra-magnifying observation, the lesion was diagnosed as EC type 3.
Despite the small size of the tumor, measuring 15 mm in diameter, the depressed configuration was clearly visible, and the findings were of type 2B in the JNET classification on the right side of the depression and of a highly atypical cancer. The findings in pit pattern diagnosis were of type VI highly irregular (invasive pattern) and of EC type 3 under ultra-magnifying observation. Although cT1b was suspected, en bloc resection was performed in diagnostic ESD due to the small size of the tumor and because the patient was of an advanced age and had underlying disease. The subsequent histopathological examination of the resected specimen showed well-differentiated adenocarcinoma, pSM1 (800 μm), BD1, Ly1, V0, HM0, VM0. The Ly factor analysis suggested that it was noncurative resection. After consultation with our surgeon, an additional operation was performed. In subsequent examinations, neither residual cancer nor lymph node metastasis was found.
* Specifications, design and accessories are subject to change without any notice or obligation on the part of the manufacturer.
Prof. Yoji Takeuchi Case 6: Colonic polyp (Tubular Adenoma)
Dr. Supakij Khomvilai
- Keyword
- Content Type